Overview
ImmuneBridge is a first-in-class integrated screening and manufacturing platform for cell therapy development.
Source
There are two main approaches for allogeneic cell therapy manufacturing and both are significantly flawed. Some companies prioritize diversity, manufacturing their products using immune cells from different donors. Some companies prioritize scalability, choosing a single heavily engineered iPSC line as the perpetual source for their cell product. Both approaches sound sufficient in theory, but in practice they each have proven risks.

Humans contain astounding amounts of genetic diversity for a reason. It enables us to survive pathogens, famines, and diverse climates. In allogeneic cell therapy trials, this donor variability even drives clinical outcomes! Patients show significantly improved progression-free survival if they receive cells from an optimal rather than suboptimal donor.1 Unfortunately, within these trials, the FDA categorizes products from distinct donors as the same “drug.” Suboptimal or inconsistent donor choice therefore muddles trial readouts, causing promising technologies to fail and ruining our ability to learn about the real biological drivers of therapeutic success or failure.
iPSCs enable developers to manufacture at true commercial scale, but they are a poor starting material and therefore fail to drive the desired clinical outcomes. This is because it is currently impossible to make iPSC-derived immune cells function comparably to the cells they are attempting to mimic. Companies are forced to layer multiple edits into these cells to compensate for their insufficient quality – a time-consuming and costly process. This means they must select a single cell line to use in perpetuity for their product, and cannot clinically evaluate multiple lines (or donors) in parallel.
The cell therapy field needs a more optimal source that can intentionally leverage donor diversity without compromising on the quantities required for commercial success. To achieve the same benefits as prior approaches, this source should be diverse, abundant, and truly scalable. We screen and expand stem cells from umbilical cord blood, adult mobilized and non-mobilized blood, or bone marrow to meet these criteria. Each source is meaningfully different from the others, and donors also vary significantly. We have learned to efficiently screen and intentionally leverage this astounding diversity – transforming variability from a flaw to a feature.
1. https://pmc.ncbi.nlm.nih.gov/articles/PMC10957466/
Screen
Cells derived from distinct donors, starting cell types, or tissues vary significantly across almost every possible attribute. Genetic and epigenetic diversity causes phenotypic and functional differences, and these in turn drive clinical outcomes. We firmly believe that diversity is a feature, not a flaw – and it can be leveraged to improve therapeutic efficacy. The challenge is finding the right combination of tissue source, donor, engineering, manufacturing process, and cell type for each therapeutic application.
We approach this massively complex problem by screening donors, engineering constructs, and manufacturing processes in high throughput using our automated and multiplexed assay system. We evaluate the critical immune functions of potential drug candidates using assays precisely matched to target patient populations – enabling us or our partners to rank and select optimal products for clinical trials and commercial manufacturing.
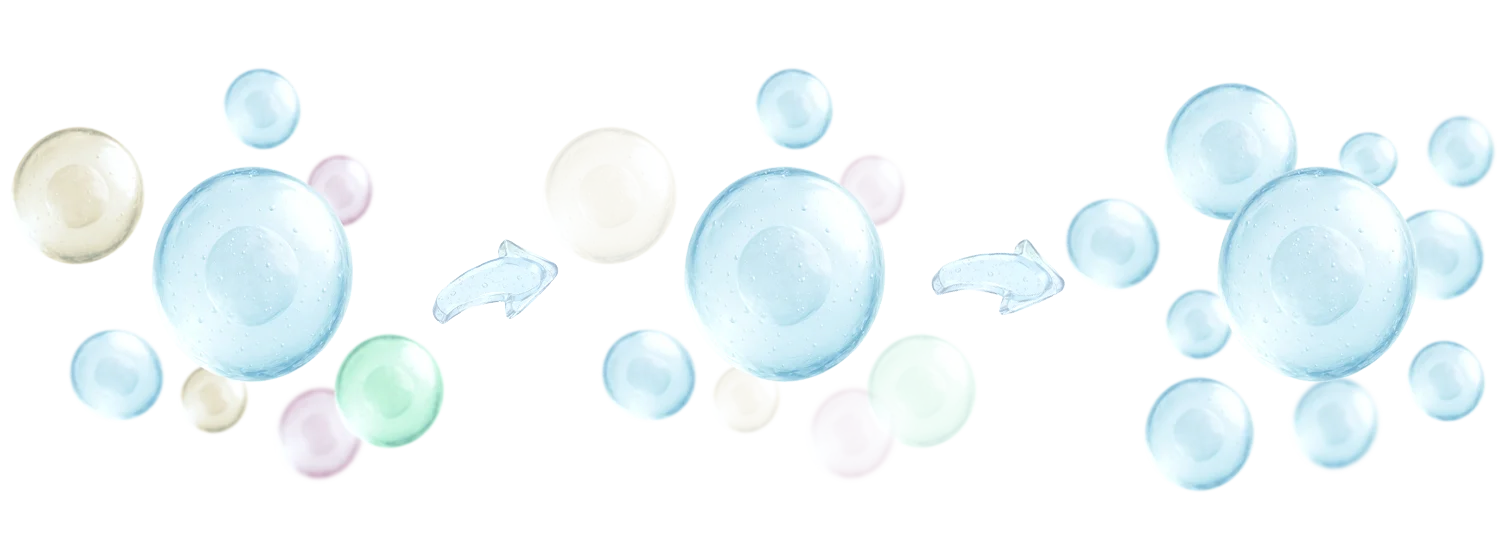
Our sample space is strikingly large – it would be costly and time consuming to test all possible combinations, despite assay automation and miniaturization. To increase efficiency, we have trained machine learning models on screening data from hundreds of donors and processes. These models can predict drug candidate performance with high accuracy using data obtained during stem cell expansion. This enables us to eliminate suboptimal candidates early in the screening process and advance only those with the best potential through immune cell differentiation, drastically increasing our throughput and decreasing screening costs.
We narrow our drug candidate pool at every stage of screening: first after initial cell production, then after in vitro assays, again after patient organoid and in vivo assays, and finally as we advance through clinical trials. This means our product efficacy continually increases throughout therapeutic development. Thanks to our unique manufacturing process, which can generate tens of thousands of doses from a single cord blood unit, best-performing candidates won’t be depleted in early clinical trial phases. Our ability to leverage clinical data to identify which candidates should advance to later stages of an adaptive trial is a major competitive advantage - many companies fail when their Phase 3 readouts don't match their Phase 1/2 efficacy, but we eliminate this failure mode. Importantly, we can train our machine learning models on clinical data to further enhance our ability to select optimal drug candidates.
Scale
Current manufacturing methods using cord blood or adult immune cells will never be able to meet commercial needs. Most companies using those cell sources can only make tens of doses per donor, causing them to rely on repeated manufacturing runs that produce inconsistent products from diverse donors. In contrast, iPSC-based manufacturing approaches can theoretically produce unlimited therapeutic doses, but their quality is suboptimal.
We have built a scalable manufacturing system to address this issue, and we can now produce tens of thousands of affordable doses of high quality immune cells from a single umbilical cord blood unit. Thanks to the hundreds of thousands of cord blood units currently cryopreserved in public banks, we can meet commercial needs for any disease. Our bioreactor-based manufacturing processes are closed, GMP-ready, feeder cell-free, and truly scalable - the methods we use to screen drug candidates are miniaturized versions of the methods we use when selectively manufacturing top performers for clinical trials at large scale.
Our manufacturing process begins with hematopoietic stem cells (HSCs), the true progenitors of all immune cells. HSCs can be easily differentiated into most immune lineages, but they aren’t commonly used because they exist at low frequencies in blood. To achieve the necessary scale, we had to solve one of the most difficult challenges in stem cell biology: inducing HSC proliferation while maintaining their multipotency.
To design a small molecule that expands HSCs without sacrificing their stemness, we carried out a massive chemical screen and extensively optimized the top hits. Our best-performing molecule is called IBR403, and it induces up to 100,000-fold proliferation in long-term culture while maintaining the ability to differentiate into lymphoid and myeloid cells. This enables us to manufacture huge stocks of HSCs as a starting material for any cellular immunotherapy - neutrophils, natural killer cells, T cells, red blood cells, macrophages or whatever else our partners want to build. HSCs are easier to engineer than mature immune cells and we can decrease reagent costs by more than 99% by modifying cells early in the HSC expansion process. This ensures that any therapy built on our platform will be affordable for the patients who need it.